In this article, we have covered ALL facts on male infertility: what percent of men are infertile, its medical and lifestyle causes, complications, and more.
Though many men shudder at the thought of a child, others desire to raise a family with their partner. In heterosexual relationships, a man who is unable to impregnate his partner is considered infertile.
This can have devastating effects on relationships or self-esteem, but the issue is typically curable. It happens for a variety of reasons – some of which we still don’t understand – and it’s happening more often now than in the 20th century.
Here are some highlights on male infertility:
- An estimated 7% of all men are affected by infertility.
- About half of male infertility cases are unexplained.
- Western infertility studies show that sperm concentration declined 52.4% from 1973 to 2011.
- Each year of age, a man’s sperm concentration decreases by 2.6%.
- 10% of all males attempting to conceive in the U.S. suffer from infertility.
- The ability of sperm to “swim” toward the egg is called sperm motility.
- About 10% of all men have varicoceles (swollen veins in the scrotum).
What Is Male Infertility?
Male infertility isn’t the same thing as erectile dysfunction. Many infertile men have no problem getting an erection, they just can’t make a baby with it.
Here’s how science defines and contextualizes male infertility:
- Infertility is a reproductive disease. It can affect men, women, or both and makes them unable to have children. In men, it means there is a reproductive problem preventing pregnancy with a female partner. (Johns Hopkins Medicine, 2019)1
- Up to 15% of reproductive-aged couples worldwide suffer from infertility. (World Health Organization, 2020)2
- Between 48 million couples and 186 million individuals around the world suffer from infertility. (World Health Organization, 2019)3
- One survey found that 52% of Americans have experienced infertility to some degree. (Single Care, 2020)4
- 10-15% of couples in the U.S. are infertile. (Mayo Clinic, 2021a)5
- About 1 in 8 couples in the U.S. are affected by infertility – that’s 6.7 million people each year. (Fertility Answers, 2020)6
What Percent of Men Are Infertile?
If you’re infertile, there’s nothing to be ashamed of – it’s a lot more common than you might think Oddly enough, the rates of male fertility and the overall sperm quality of the male population are decreasing.
Science is still figuring that one out, but in the meantime, here are the numbers on male infertility:
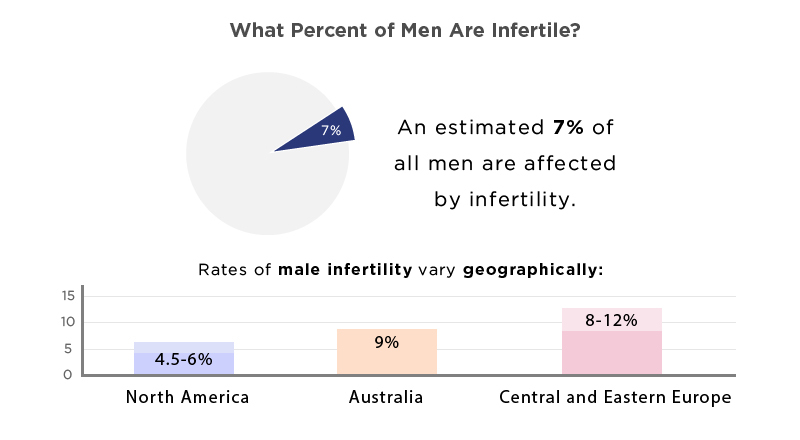
- Rates of male infertility vary geographically: (Reproductive Biology and Endocrinology, 2015)7
- North America – 4.5-6% male infertility.
- Australia – 9% male infertility.
- Central and Eastern Europe – 8-12% male infertility.
- 10% of all males attempting to conceive in the U.S. suffer from infertility. (Cleveland Clinic, 2021)8
- An estimated 7% of all men are affected by infertility. (Newcastle University, 2022)9
- 50% of fertility problems in heterosexual couples are caused by the male’s infertility. (Newcastle University, 2022)9
- About half of male infertility cases are unexplained. (Newcastle University, 2022)9
- About 40-50% of all infertility cases are due to male infertility. As many as 2% of men will have suboptimal sperm. It may be due to low sperm concentration, poor sperm motility, unusual morphology, or a combination. (Journal of Human Reproductive Sciences, 2016)10
Male Fertility Is Declining
We mentioned it before, but the declining rate of male fertility is worth taking a deep dive into. Humans really only started counting their sperm in the 20th century, so there’s no good way to know if it’s been declining forever or if this is a recent development.
Either way, research suggests that men are steadily becoming less and less fertile. Here’s the data:
- From 1940 to 1990, the mean seminal volume of men decreased from 3.40 mL to 2.75 mL, with an estimated change of -0.0130 mL annually. (BMJ Clinical Research, 1992)11
- Smaller semen volumes impact fertility; if there isn’t enough fluid to bring sperm to the egg, it won’t be fertilized. (IVF Plano, 2013)12
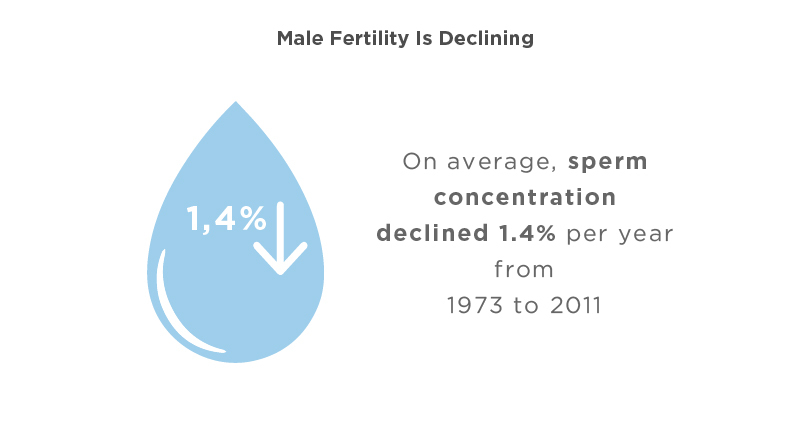
- On average, sperm concentration declined 1.4% per year (52.4% overall) from 1973 to 2011 in Western infertility studies. (Human Reproduction Update, 2017)13
- From 1973 and 2011, studies of Western men (who had never had a child) showed a 50-60% decline in sperm count. (Human Reproduction Update, 2017)13
- The proportion of men with normal total motile sperm counts declined by about 10% from 2002 to 2017. (Urology, 2019)14
- Low sperm count means there are fewer sperm than normal when a man ejaculates. Less than 15 million sperm per mL of semen is low. This decreases the odds of pregnancy but doesn’t make it impossible. (Mayo Clinic, 2020)15
Causes of Male Infertility and Associated Medical Conditions
Infertility can be caused by anything from diabetes to testicular cancer to cigarettes. If you don’t want to risk having a kid, now might be a good time to take up smoking.
Here are the conditions and lifestyle choices that cause infertility:
- Low sperm production, abnormal sperm function, or blockages in sperm delivery can all cause male infertility. Certain illnesses, injuries, chronic health issues, lifestyle choices, and other factors may also contribute. (Mayo Clinic, 2021b)16
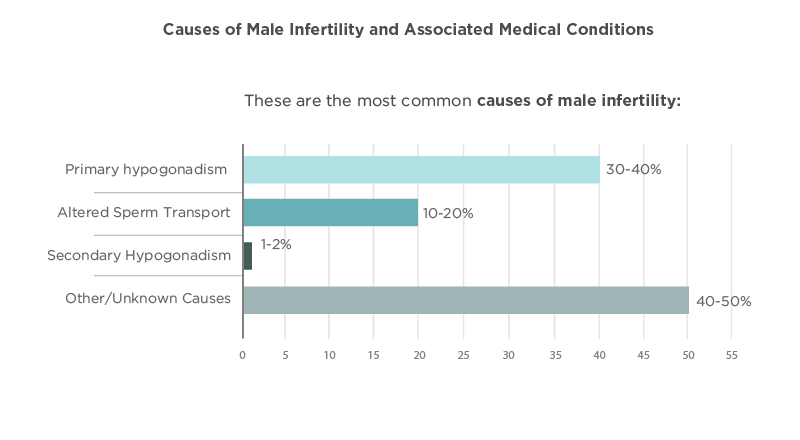
- These are the most common causes of male infertility: (CNY Fertility, 2022)17
- Primary hypogonadism – 30-40%
- Androgen Sensitivity
- Androgen Excess State
- Estrogen excess state
- Congenital or developmental testicular disorder (e.g., Klinefelter syndrome)
- Medication
- Radiation
- Testicular Trauma
- Varicocele
- Altered Sperm Transport – 10-20%
- Obstruction of the reproductive tract
- Hormonal disorders
- Failure to produce sperm
- Poor sperm function and quality
- Secondary Hypogonadism 1-2%
- Androgen excess state (e.g., tumor, exogenous administration)
- Congenital idiopathic hypogonadotropic hypogonadism
- Estrogen excess state (e.g., tumor)
- Infiltrative disorder (e.g., sarcoidosis, tuberculosis)
- Medication effect
- Multiorgan genetic disorder (e.g., Prader-Willi syndrome)
- Pituitary adenoma
- Trauma
- Other/Unknown Causes – 40-50%
- Diet
- Exposure to toxins
- Smoking/drinking/marijuana use/other lifestyle choices
- Heat
- Cancer
- Testicular Failure
- Unknown
- Primary hypogonadism – 30-40%
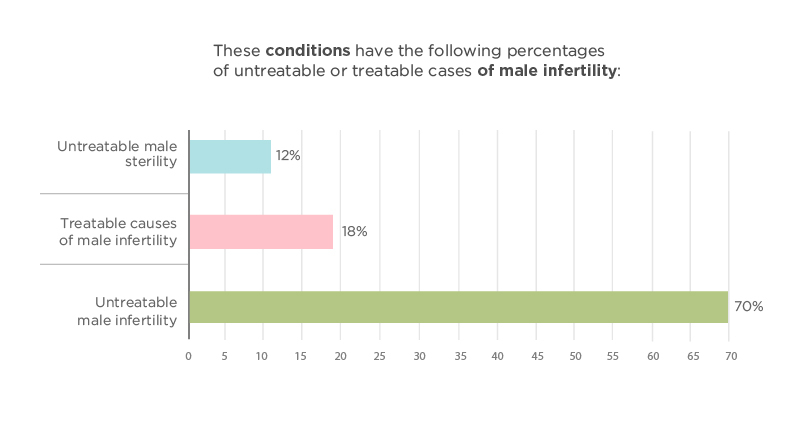
- These conditions have the following percentages of untreatable or treatable cases of male infertility: (StatPearls, 2022)18
- Untreatable male sterility is seen in 12% of cases with these conditions:
- Primary seminiferous tubular failure
- Sertoli cell-only syndrome
- Bilateral orchiectomy
- Treatable causes of male infertility are found in 18% of cases involving these conditions:
- Obstructive azoospermia
- Ejaculatory duct cysts
- Prostatic midline cysts
- Gonadotropin deficiency
- Sexual function disorders
- Sperm autoimmunity
- Varicoceles
- Reversible toxin effects.
- Untreatable male infertility is found in 70% of cases with these conditions, and assisted reproductive technology is required to conceive.
- Oligozoospermia
- Asthenozoospermia
- Teratozoospermia
- Normospermia with functional defects
- Untreatable male sterility is seen in 12% of cases with these conditions:
- Some of the most common conditions and disorders associated with male infertility are as follows: (StatPearls, 2022)18
- Adult growth hormone deficiency
- 5-Alpha reductase deficiency
- Androgen receptor gene polymorphisms
- Brain damage from tumors or trauma
- Bilateral testicular torsion
- Celiac disease (associated with androgen resistance)
- Chemotherapy (especially alkylating agents such as cyclophosphamide)
- Chromosomal abnormalities (Y chromosome microdeletions in azoospermic regions AZFa, AZFb, and AZFc)
- Congenital adrenal hyperplasia (32-hydroxylase deficiency)
- Cryptorchidism
- Cushing disease
- Cystic fibrosis
- Down syndrome
- Drug use (even commonly prescribed medications such as cimetidine, spironolactone, tetracycline, nitrofurantoin, sulfasalazine, and calcium channel blockers)
- Ejaculatory duct obstruction
- Estrogen excess
- Follicle-stimulating hormonal (FSH) abnormalities
- FSH receptor gene mutation
- Hemochromatosis
- Hodgkin lymphoma (due to the need for extensive chemotherapy)
- HIV infections (causes low sperm motility)
- Human beta-defensin abnormalities
- Hypogonadotropic hypogonadism
- Hypogonadism
- Hypopituitarism
- Immotile cilia syndrome
- Kallmann syndrome
- Kartagener syndrome
- Klinefelter syndrome
- Lead exposure
- Leprosy
- Liver failure
- Luteinizing hormone (LH) deficiency
- Marijuana associated disorders
- Mixed gonadal dysgenesis
- Mumps
- Myotonic dystrophy
- Noonan syndrome (male Turner syndrome)
- Obesity
- Opioid abuse
- Pesticide, fungicide, and chemical exposure
- Pituitary adenomas, prolactinomas
- Primary hypogonadism
- Prostate and pelvic surgery
- Radiation exposure (Sertoli and sperm cells are much more sensitive than Leydig cells)
- Recurrent urinary tract infections
- Renal failure
- Reifenstien syndrome (partial androgen insensitivity)
- Sarcoidosis
- Seminomatous and non-seminomatous germ cell testicular tumors
- Sex reversal syndrome
- Sertoli cell-only syndrome (azoospermia with high FSH levels. Testis biopsy needed for diagnosis.)
- Sickle cell anemia (due to intratesticular ischemia)
- Smoking
- Spinal cord injury
- Sexually Transmitted Diseases (STDs)
- Testicular cancers
- Testicular torsion
- Testicular trauma
- Testosterone supplementation
- Thalassemia
- Tuberculosis
- Thyroid disorders
- Tuberculosis
- Urethral infection, stricture, or trauma
- Varicoceles
- Young syndrome
- An estimated 0.3% of men attending infertility clinics have diabetes mellitus, and about 1% of subfertile males may have diabetes. Diabetics may also experience failure of emission, and calcification of the vas deferens happens 6 times as frequently in diabetics.
- Testicular Cancers:
- Testicular germ cell tumors may cause semen abnormalities leading to male infertility. (Journal of Adolescent and Young Adult Oncology, 2014)19
- In testicular cancer patients, semen abnormalities are present even before treatment begins. (Stony Brook Medicine, n.d.)20
- Problems with making and growing sperm may cause sperm to exhibit the following abnormalities: (Urology Care Foundation, n.d.)21
- Not grow fully
- Be oddly shaped
- Not move the right way
- Be made in very low numbers (oligospermia)
- Not be made at all (azoospermia)
- Testicular cancer may cause sperm abnormalities for the following reasons: (Stony Brook Medicine, n.d.)20
- Local pathological changes in the contralateral testis after orchiectomy (Sertoli cell only syndrome, fibrosis, carcinoma in situ)
- Antisperm antibodies (21-77% of patients)
- Endocrine factors (elevation of beta GCG and alpha-fetoprotein, Estradiol, LH, and low serum testosterone).
- Increase intrascrotal temperature and functional/structural changes in the epididymis secondary to a change in blood flow
- In developed countries, abnormal semen production is thought to be the cause of up to 50% of all infertilities. (Journal of Reproduction & Infertility, 2012)22
- Varicoceles
- Varicoceles are swollen scrotum veins present in 16 out 100 of all men. 40 out of100 infertile men have them. They block blood drainage and make testicles too warm, harming the sperm. (Urology Care Foundation, n.d.)21
- About 10% of all men have varicoceles. In infertile couples, incidence increases by 30%. They are most common in men aged 15-35, and between 70,000-80,000 American men undergo surgery to correct them annually. (UCSF Department of Radiology & Biomedical Imaging, 2010)23
- Smoking
- 36.4% of studies comparing smokers to non-smokers reported a significant reduction in sperm motility and concentration, and 41.4% showed a decrease in normal morphology. (The World Journal of Men’s Health, 2015)24
- Smoking affects sperm motility by 40%, concentration by 30%, and morphology by 42.1%. (The World Journal of Men’s Health, 2015)24
- Smoking over 10 cigarettes per day can reduce sperm concentration by 13-17%. (Fertility and Sterility, 1994)25
- Obesity/Overweight/Underweight
- Odds of infertility increase by 10% for every 20 lbs (9 kg) a man is overweight. (Central European Journal of Urology, 2015)26
- A Danish study found that men with a body mass index (BMI) less than 20 kg/m2 had 28.1% reduced sperm concentration and 36.4% reduced sperm count. (Fertility and Sterility, 2004)27
- The same study found that men with a BMI over 25kg/m2 had a 21.6% reduced sperm concentration and 23.9% reduced sperm count. (Fertility and Sterility, 2004)27
Complications of Infertility in Men
Wanting a family is (usually) one of the purest and most beautiful feelings in the human experience. However, when a couple is denied children – through no fault of their own – it can cause serious psychological damage and relationship strain.
Here are the recorded complications, costs, and psychological effects of male infertility:
- Psychological distress, stress, and marital issues can be caused by infertility. In the U.S., infertility treatments can be expensive, are not often covered by insurance, and are not guaranteed to succeed. (StatPearls, 2022)18
- Male infertility can cause several complications, including: (Mayo Clinic, 2021b)16
- Stress and relationship difficulties related to the inability to have a child.
- Expensive and involved reproductive techniques.
- Increased risk of testicular cancer, melanoma, colon cancer, and prostate cancer.
- A British study found that 93% of respondents said their well-being had been affected by infertility, leading to poor mental well-being and self-esteem issues. (Fertility Network UK, 2017)28
- One survey of infertile U.S. adults found that 83% reported that infertility affected their mental health and/or relationships (Single Care, 2020)4
- One survey found that 86% of those who had to undergo infertility treatment said they passed up options that their doctor recommended or were only considering it due to the cost. (CoFertility, 2021)29
- A survey of Americans undergoing fertility treatment found that the following percentages of respondents estimated spending these amounts of money on treatments by the time they were finished: (CoFertility, 2021)29
- Over $100,000 – 8%
- $50,000 – $99,999 – 28%
- $25,000 – $49,999 – 18%
- $10,000 – $24,999 – 17%
- Under $10,000 – 28%
Male Fertility and Age
Lots of things get harder with age, but the penis isn’t one of them. As a man gets older, his sperm production gets weaker.
The chances of a healthy pregnancy decrease with age. Here’s the data:
- Couples with a male partner over 40 are more likely to have difficulty conceiving. (Centers for Disease Control and Prevention, 2018)30
- Sperm quality decreases around ages 40-45. As male age increases, the chance of pregnancy decreases, and the risks of miscarriage and fetal death increase. (Better Health, n.d.)31
- Sperm motility is the ability of the sperm to move properly toward the egg. (Extend Fertility, 2018)32
- One study found that male sperm motility decreased by 0.8% per year of age. (Human Reproduction, 2008)33
- Sperm morphology is the sperm’s shape, including the head, midpiece, and tail structure. The head is important as it can affect the sperm’s ability to penetrate and fertilize the egg. (Loma Linda University, 2017)34
- Each year of age, a man’s sperm morphology decreases by about 0.65%. (Legacy, 2021)35
- Sperm Count is the number of sperm per ejaculation. Low sperm counts decrease the chance of pregnancy. (Legacy, 2021)35
- Each year of age, a man’s sperm concentration decreases by 2.6%. (New England Journal of Medicine, 1995)36
Signs and Symptoms of Male Infertility
While male infertility doesn’t always present with any symptoms at all, there are some cases where it does.
If you have a symptomatic male infertility condition, the good news is that the symptoms will be very, very apparent. The bad news is that they include male breast growth and testicle swelling.
- The primary sign of male infertility is the inability to have a child – there might be no other obvious symptoms. (Mayo Clinic, 2021b)16
- In some cases, a problem such as an inherited disorder, hormonal imbalance, dilated veins around the testicles, or blockage of sperm may cause symptoms including: (Mayo Clinic, 2021b)16
- Problems with sexual function — for example, difficulty with ejaculation or small volumes of fluid ejaculated reduced sexual desire, or difficulty maintaining an erection (erectile dysfunction).
- Pain, swelling, or a lump in the testicle area.
- Recurrent respiratory infections.
- Inability to smell.
- Abnormal breast growth (gynecomastia).
- Decreased facial or body hair or other signs of a chromosomal or hormonal abnormality.
- A lower than normal sperm count (fewer than 15 million sperm per milliliter of semen or a total sperm count of less than 39 million per ejaculate).
Conclusion
The best data shows male infertility affects about 7% of all men, but not all men are trying to have children, so this number may be much higher. Many conditions can cause infertility, but a large number of cases remain unexplained.
Around the world, male fertility has been steadily declining for generations. Though there is no clear answer as to why, researchers hypothesize a combination of increased obesity rates, environmental toxins, and poorer diets.
Male infertility can cause serious distress to couples who want to have children. It can lower a man’s self-esteem and harm his mental well-being. While treatments are available and often successful, they can be costly – especially in the U.S.
While many causes of the disease can’t be prevented, others can. Living an active lifestyle, committing to a healthy diet, and staying away from cigarettes are all ways to reduce the risk of male infertility.
At the end of the day, if you’re doing everything you can and nothing is working, seek treatment. If treatment isn’t an option, keep trying – many couples who don’t conceive in the first year have success in the subsequent year, and adoption is also an option.
Infertility can be debilitating and frustrating, but it doesn’t have to prevent men from starting a family.
Footnotes
- Johns Hopkins Medicine, 2019. A medical article on the disease called infertility and how it presents in men.
- World Health Organization, (Archived) 2020. An article on the worldwide prevalence of infertility and how it affects people.
- World Health Organization, 2019. An overview of available data on infertility worldwide and the numbers of people it affects.
- Single Care, 2020. An article on the lack of fertility awareness and the effectiveness of treatments using data from a survey of 600 Americans.
- Mayo Clinic, 2021a. An article on the characteristics of infertility, including its prevalence, symptoms, and treatment options.
- Fertility Answers, 2020. An article on infertility statistics, the characteristics of infertility, and its common causes.
- Reproductive Biology and Endocrinology, 2015. A study of 16 academic articles related to the prevalence of male infertility worldwide.
- Cleveland Clinic, 2021. An article on the prevalence of male infertility, its common causes and symptoms, and its potential treatments.
- Newcastle University, 2022. An article on a scientific breakthrough that discovered a genetic mechanism that can cause male infertility.
- Journal of Human Reproductive Sciences, 2016. A medical article analyzing male infertility trends around the globe using data from a variety of sources.
- BMJ Clinical Research, 1992. A study on 61 different articles relating to male infertility that identifies a global decrease in semen quality.
- IVF Plano, 2013. An article on male infertility and the various characteristics of semen that can cause it to be less fertile.
- Human Reproduction Update, 2017. A study of semen from 42,935 men who gave samples across 429 studies from 1973 to 2011.
- Urology, 2019. A study of semen analyses from 119,972 men in subfertile couples to determine their motile sperm counts.
- Mayo Clinic, 2020. An article on low sperm counts in men, the symptoms associated with the condition, and when to seek treatment.
- Mayo Clinic, 2021b. An article on infertility in men, the symptoms associated with the condition, and when to seek treatment.
- CNY Fertility, 2022. An article on the prevalence of infertility and its various medical causes for men and women.
- StatPearls, 2022. A journal article on male infertility and the plethora of conditions that cause it, both treatable and untreatable.
- Journal of Adolescent and Young Adult Oncology, 2014. A study of 6 different publications related to semen abnormalities and testicular cancer.
- Stony Brook Medicine, n.d. An article on the medical conditions associated with male infertility.
- Urology Care Foundation, n.d. An article on male infertility, its many causes, sperm disorders, and treatments.
- Journal of Reproduction & Infertility, 2012. A study on male infertility and the pharmaceutical medications that may affect it.
- UCSF Department of Radiology & Biomedical Imaging, 2010. An article on the non-surgical treatments available for infertility caused by varicoceles.
- The World Journal of Men’s Health, 2015. A study of 33 separate studies on the link between cigarette smoking and semen quality.
- Fertility and Sterility, 1994. A study on the effect of cigarette smoking on a man’s sperm quality.
- Central European Journal of Urology, 2015. A study on the different mechanisms linking obesity to male infertility.
- Fertility and Sterility, 2004. A study on the relationship between body mass index and reproductive hormones in 1,558 Danish men.
- Fertility Network UK, 2017. A study of 41 men’s experiences with infertility in the U.K. and how it affected their lives.
- CoFertility, 2021. A survey of 858 American needing infertility treatment on how much they had to pay for medical care.
- Centers for Disease Control and Prevention, 2018. A FAQ section from the CDC on infertility and its causes.
- Better Health, n.d. An informative article on the relationship between age and fertility.
- Extend Fertility, 2018. An article on the prevalence and causes of male infertility and how to test for it.
- Human Reproduction, 2008. A study examining the relationship between male age and sperm motility using data from 90 non-smoking men aged 22-80.
- Loma Linda University, 2017. An article on the shape and size (morphology) of sperm, its different types, and its effect on fertility.
- Legacy, 2021. An article on the physiological ways that a man’s age impacts the characteristics of his sperm and fertility.
- New England Journal of Medicine, 1995. A study of sperm count and fertility among 1,351 healthy men in Paris.